A long long long time and many microscopes ago...
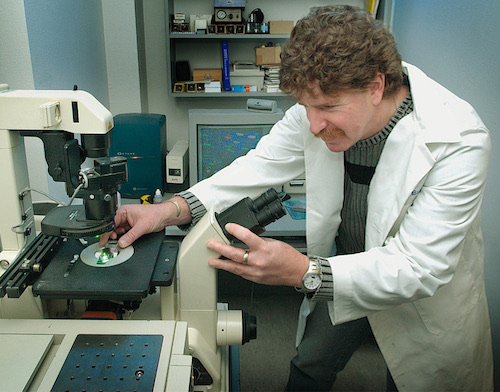
Dr. Mark Sussman is a Distinguished Professor of Biology at San Diego State University and key investigator at the San Diego State University Heart Research Institute. Upon completing his doctoral thesis at the University of Southern California where he studied viral immunology in 1989, Dr. Sussman entered myocardial research though postdoctoral studies in cytoskeletal biology characterizing the role of the actin filament capping protein tropomodulin in heart under the mentorship of Dr. Larry Kedes. In 1995, Dr. Sussman accepted a position as Assistant Professor in the Division of Molecular and Cardiovascular Biology at Children’s Hospital Medical Center in Cincinnati, Ohio. Building upon his postdoctoral work, Dr. Sussman created the first mouse model of dilated cardiomyopathy, which exhibited myofibril organizational defects resulting from cardiac-specific transgenic overexpression of tropomodulin. Over his ensuing eight year tenure at Children’s Hospital, his lab completed more than a dozen published studies examining the multiple facets of the pathogenesis of dilation in the tropomodulin mouse model including calcium handling abnormalities, cytoskeletal defects, and altered signal transduction. Additional studies on myocardial signal transduction involving the small GTPase rac1 produced another murine model of cardiomyopathy and prompted Dr. Sussman to examine molecular interventional strategies to inhibit the progression of dilation and heart failure. Intrigued by prevailing paradoxical observations in published literature linking the cardioprotective kinase Akt/PKB to heart failure in transgenic mouse models, Dr. Sussman found nuclear accumulation of Akt/PKB in response to anti-apoptotic stimuli. These seminal observations led to Dr. Sussman’s pioneering studies relating Akt/PKB and gender as he demonstrated myocardial differences between the sexes in Akt/PKB nuclear accumulation that stem from estrogenic stimuli. This finding was the genesis of his pivotal contribution to survival signaling networks in heart: targeting of Akt/PKB to the cardiomyocyte nucleus affords cardioprotection without deleterious hypertrophic consequences. Fusing his ongoing studies of cardioprotection together with his background in cytoskeletal biology, Dr. Sussman expanded his studies of nuclear Akt/PKB biology to include novel associations with LIM domain proteins that shuttle through the nucleus. His Akt/PKB-related research involves surprising effects of nuclear Akt/PKB signaling for cardiomyocytes including anti-hypertrophic signaling, induced downstream mediators of cell survival including Pim-1 kinase, and the potentiation of survival and regenerative capacity for cardiac stem cells. These studies have been published in high impact journals including the Journal of Clinical Investigation, Proceedings of the National Academy of Sciences, Nature Medicine, Circulation Research, Nature Communications, the Journal of the American College of Cardiology, and many more.
Repairing and restoring myocardial structure and function represents the ideal outcome for treatment of cardiomyopathy. Current therapeutic interventions rely predominantly upon pharmacologic strategies to slow the progression of heart failure, but the ultimate destination for many of these patients will be an operating room where they will receive a mechanical assist device or a transplanted donor heart. The cost, invasiveness, shortage of suitable donor organs, and compromised quality of life are just a few of the many issues stemming from the current approaches to treatment of heart failure. An attractive alternative vision for these patients would be the use of repair processes that, rather than prop up and maintain damaged organ function, would enable the replacement and repair of the compromised tissue on a cellular level. Over the past decade a concerted effort by scientists and clinicians has advanced the use of gene therapy as an approach to treatment of heart failure. These studies have shown that genetic reprogramming of the myocardium can be used to prevent cell death, inhibit maladaptive remodeling, enhance hemodynamic function, promote angiogenesis, and block deleterious signaling. Although gene therapy approaches remain a popular avenue for delineating the role of proteins in cardiac repair and rescue, many practical aspects of gene therapy such as delivery and targeted expression in the myocardium, regulation of gene expression, and persistence of expression have hampered implementation of myocardial gene therapy for treatment of heart failure. However, recent discoveries related to regeneration and repair of the myocardium have shifted the paradigm of treatment for myocardial disease. Discoveries linking cell-based therapies to improvements in myocardial performance have invigorated the field, but current limitations in cell-based approaches present significant barriers.
Recently, Dr. Sussman has become interested in the cardiopulmonary effects of vaping and consequences for the heart and lungs. He has embarked upon novel studies to assess the biology of vaping using mouse and rat models. Dramatic increases in use of flavored vaping juices among young people, the incredibly addictive impact of nicotine-salts in vape fluids, recent legalization of marijuana, and expanding use of cannabinoid-derived compounds for medicinal purposes are all compelling reasons to pursue research in this expanding area. Equipment in the Sussman lab enables rodent inhalation studies using commercially available vape pens, e-cigarettes, and conventional cigarettes to produce experimental models that mimic real-world conditions. These studies are supported with funding from the California Tobacco-Related Disease Research Program.
Dr. Sussman’s research has been supported by grant awards from the National Institutes of Health and the American Heart Association since establishing his independent laboratory in 1995. He was recognized as an Established Investigator of the National American Heart Association in 2000. Dr. Sussman served on multiple leadership and review committees for the American Heart Association at both affiliate and national organization levels. He has authored over 200 peer-review articles and is a popular speaker at national and international venues with over 230 invited presentations in the last 20 years. Dr. Sussman also served as Chair of the study section for Cardiac Contractility, Hypertrophy, and Heart Failure at the National Institutes of Health from as well as a standing member of editorial boards for several journals including Circulation Research, the Journal of Biological Chemistry, the American Journal of Physiology (Heart and Circulatory Physiology), Regenerative Medicine, and the Journal of Molecular and Cellular Cardiology. His laboratory at San Diego State University serves as a training ground for undergraduate, masters and doctoral students, and postdoctoral trainees who are now mentored under Dr. Sussman’s guidance. He championed efforts to bring together cardiovascular researchers in the San Diego academic community with a collaborative research Program Project Grant that pooled knowledge and resources to further studies on the molecular and cellular basis of heart failure – the first award of its kind for any California State University campus. In addition to the Program Project Grant award, Dr. Sussman was also the recipient of a MERIT award, multiple independent investigator awards from the NIH, a principal investigator in a Fondation Leducq Transatlantic Networks of Excellence Program, as well as serving as co-principal investigator in the SDSU/UCSD Cancer Center Comprehensive Partnership.
A short biographical article detailing Dr. Sussman’s journey to become a cardiovascular researcher and philosophical musings on a career in scientific research can be found as a PDF file by clicking on this link: sussman-bio
Dr. Sussman’s favorite self-authored opinion article describing his viewpoint of surviving in science and the danger of having an opinion can be found by clicking on this link: A Matter of Opinion

